Inflammatory Myopericardial Syndromes (IMPS)
ESC 2025 terminology covering the spectrum from pericarditis → myopericarditis → myocarditis. A frequent mimic of MINOCA.
1) Spectrum & Causes
The IMPS spectrum
- Pericarditis – inflammation of the pericardium; chest pain worse lying flat; friction rub; effusion possible.
- Myopericarditis – predominantly pericardial with mild myocardial involvement (troponin rise ± subtle LV impairment).
- Myocarditis – predominantly myocardial; LV dysfunction/arrhythmia risk higher; may present like an acute coronary syndrome.
Common causes
- Viral/post-viral syndromes and post-infective immune responses
- Autoimmune/rheumatological disease; post-autoimmune flare
- Drug reactions/toxins (rare); hypersensitivity
- Systemic inflammatory disorders
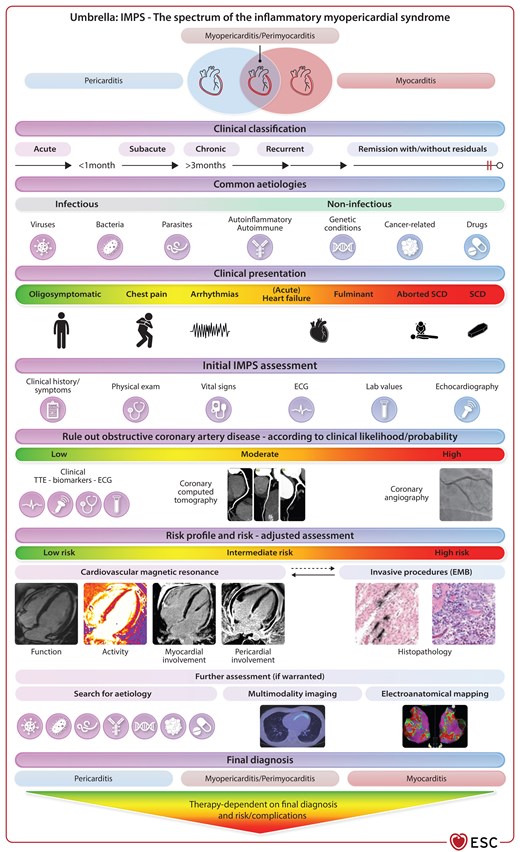
Guideline-based overview
The European Society of Cardiology (ESC) 2025 guidance recognises Inflammatory Myopericardial Syndromes (IMPS) as a spectrum from isolated pericarditis to myocarditis and overlapping forms. The figure below (ESC central illustration) summarises classification, diagnostic work-up and risk-adjusted management pathways.
Source: European Heart Journal, doi:10.1093/eurheartj/ehaf192.
2) Diagnostic pathway (aligned with ESC 2025)
Initial triage
- History & examination (pleuritic/positional pain? viral prodrome?)
- 12-lead ECG (diffuse concave ST ↑, PR ↓; arrhythmias)
- High-sensitivity troponin; CRP/ESR; FBC, U&E, LFT
- Rule out obstructive CAD if ACS is suspected (angiography/CTCA)
Core imaging
- Echocardiography: LV/RV function, pericardial effusion
- CMR (key): T2 oedema mapping; non-ischaemic LGE; pericardial enhancement
- CMR differentiates IMPS from infarction in suspected MINOCA
Selected tests
- Autoimmune/viral serology guided by clinical context
- Holter/patch monitoring for palpitations or syncope
- Endomyocardial biopsy in fulminant/atypical cases (specialist centres)
Not all tests are required for everyone; plans are individualised.
3) Management
3.1 Non-pharmacological
- Temporary activity restriction beyond sedentary levels until clinical remission (symptoms resolved; CRP/troponin normal; ECG stable; no active inflammation on CMR where performed). Duration is individualised; many need ≥1 month, longer if myocardial involvement.
- Gradual, supervised return to work and exercise; cardiac rehabilitation and psychological support are helpful.
3.2 Pericarditis-predominant
- Empirical anti-inflammatory therapy (aspirin/NSAID) plus colchicine to reduce recurrences; PPI gastro-protection when needed.
- Low-to-moderate dose corticosteroids only when first-line therapy is contraindicated or ineffective; taper slowly once in remission.
- Recurrent/incessant cases: consider IL-1 blockade (e.g., anakinra or rilonacept) in specialist care to reduce steroid exposure; other options in selected cases.
- Monitor CRP and, in complex cases, CMR to guide duration and tapering.
3.3 Myopericarditis / Myocarditis-predominant
- Supportive care with guideline-directed heart failure therapy when LV function is impaired; beta-blockers often used in practice.
- Pain control with aspirin/NSAID as needed; colchicine is safe in myopericarditis to prevent recurrences.
- Specific aetiologies (e.g., eosinophilic, giant-cell, sarcoidosis, ICI-associated, Lyme, Chagas) require targeted immunosuppression or anti-infective therapy in expert centres.
- Arrhythmia assessment and management; device therapy according to risk and guidelines.
3.4 Fulminant myocarditis & advanced support
- Early recognition of shock; prompt transfer to tertiary centres for temporary mechanical circulatory support (commonly VA-ECMO) where indicated.
- Early biopsy can inform aetiology-directed immunosuppression in non-infective forms.
3.5 Interventional & surgical options
- Pericardiocentesis for tamponade or large symptomatic effusions; drainage usually guided by echo/fluoroscopy.
- Selected procedures (balloon pericardiotomy; intrapericardial therapies) in refractory cases at experienced centres.
- Pericardiectomy for chronic constrictive pericarditis not responding to medical therapy—preferably in high-volume centres.
- Refractory myocarditis: durable LVAD or heart transplantation may be considered when recovery is not achievable.
3.6 Arrhythmias & sudden cardiac death prevention
- Risk-stratify using symptoms, ECG, ambulatory monitoring and CMR (extent/location of LGE).
- Wearable defibrillator may be considered short-term in higher-risk cases; ICD decisions are typically revisited after 3–6 months of follow-up when inflammation has settled.
4) Follow-up, return-to-exercise & red flags
Follow-up schedule
- Review at 6–12 weeks; repeat echo if initial LV impairment
- CMR at 3–6 months for myocarditis or persistent symptoms
- Holter/stress testing where arrhythmia risk is suspected
Return-to-exercise
- Pericarditis: gradual return once pain and CRP have normalised
- Myopericarditis/myocarditis: usually ≥3–6 months; require symptom resolution, normal biomarkers and no significant arrhythmias
- Athletes: follow sports-cardiology protocols
Red-flag symptoms
- Severe/worsening chest pain, new breathlessness or fainting
- Palpitations with dizziness/blackouts; sustained rapid/irregular heartbeat
- Fever not settling; leg swelling; signs of heart failure
If acutely unwell, call 999 or attend the Emergency Department.
5) Why IMPS can look like a heart attack (MINOCA)
- Chest pain, ECG changes and troponin rise overlap with acute coronary syndromes
- Coronary arteries are non-obstructed; diagnosis relies on CMR patterns and clinical context
- Early comprehensive testing reduces misclassification and unnecessary invasive procedures
6) Prognosis
Most people with uncomplicated pericarditis or myopericarditis have a good outlook…
7) Knowledge gaps & research priorities
- Predictors of relapse and optimal duration of colchicine
- Risk stratification for arrhythmias when myocarditis is MRI-only
- When/how to use immunosuppression in non-infective IMPS
- Exercise prescription and return-to-play frameworks across the spectrum
Read the ESC guidance: 10.1093/eurheartj/ehaf192
8) Quick FAQs
- Can IMPS come back? Yes. Recurrence is possible, especially in pericarditis; colchicine lowers risk.
- Can I exercise? Yes, but timing depends on phenotype; follow the return-to-exercise advice above.
- Is this a heart attack? No – symptoms can mimic a heart attack, but arteries are not blocked.